Serendip is an independent site partnering with faculty at multiple colleges and universities around the world. Happy exploring!
The Prenatal Causes of Schizophrenia
Schizophrenia is a mental illness affecting nearly 2.2 million Americans (5) or 0.5% (3) people world wide. Although this is a relatively low prevalence rate, it is a very debilitating disease which still has no known cure or direct cause. By studying the histories and symptoms of current schizophrenic patients, more can be learned about the disease to help future victims.
Symptoms usually develop between 15-25 years old for men and between 25-35 years old for women (3) and are characterized by both positive and negative symptoms. Positive symptoms include auditory hallucinations, olfactory hallucinations (unpleasant smells), gustatory hallucinations (unpleasant tastes), somatic hallucinations (pain), visual hallucinations, delusions and loosening of associations or “word salad” (3). Negative symptoms are those which affect normal functioning. These include avolition, poverty of speech, or even catatonia (3). Patients who suffer from primarily positive symptoms are said to have acute schizophrenia, while those who suffer from primarily negative symptoms are said to have chronic schizophrenia.
Many factors are responsible for the development of schizophrenia. Though the causes of schizophrenia are still not fully known, researchers are aware that it is a combination of genetic, biological and environmental factors (3). Biological and genetic factors play a large role in the manifestation of the disease. There is a significant genetic risk factor associated with schizophrenia. Parents and siblings of schizophrenics have a 10 times increased risk factor for developing schizophrenia, while children of schizophrenics have a 15 times higher risk factor. In mono-zygotic twin studies, there is a 53% chance that if one twin is schizophrenic that the other will be and in di-zygotic twins there is a 15% concordance rate. This shows there is a high genetic hereditability piece involved in schizophrenia (3). Unlike other mental disorders which show predominantly environmental risk criteria or biological risk criteria, schizophrenia is unique in having both sectors be important.
Several prenatal factors including time of birth, place of birth, infections during pregnancy, malnourishment, stress, and rhesus incompatibility have been implicated in the causation of schizophrenia (1). There is 5-8% excess of births of babies born in the winter/spring that later develop schizophrenia or manic/depressive disorder. There is a significant correlation between urban births and schizophrenia. Both of these factors, urban environment and winter/spring birth could be associated with the higher prevalence of infections present in both settings (1).
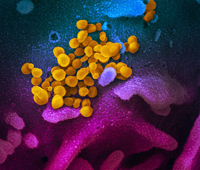
There are several prenatal factors which increase the risk of developing schizophrenia. Respiratory infections including influenza, pneumonia, tuberculosis and acute bronchitis all lead to an increased risk for schizophrenia. There has also been evidence that exposure to viruses and polio during pregnancy also increases the chances of schizophrenia (1). The Prenatal Determinants of Schizophrenia (PDS) was a study conducted in the 1990s using previously gathered maternal sera samples from 20,000 women in California. The sera was frozen and then used in conjunction with hospital records and diagnostic criteria to ultimately trace 71 cases of schizophrenia. Due to the previous research on the link between influenza and schizophrenia, the sera was tested for prevalent strains of influenza. Most women involved in the study only had three sera samples taken, one each trimester. The researchers found that “first trimester exposure was associated [with] a 7-fold increase in risk of schizophrenia and SSDs, whereas second and third trimester exposure showed no increase in risk” (4). This is quite a large increase and shows a direct correlation between early gestational exposure in influenza and the development of schizophrenia.
Malnourishment may also play a role in the development of schizophrenia. Traditionally, it has been thought that fetuses that were exposed to malnourishment early in gestation but not during late gestation have a much higher rate of schizophrenia (1). The same PDS study also examined the nourishment, but instead of looking at low weight, they examined high weight. They found a significant increase in the prevalence of schizophrenia and high BMI (4). Although this data disputes the previously known data, it also shows that “unhealthy” mothers, be them too heavy or too thin, do not carry as healthy children as those women who are a healthier weight.
Stress may also increase the likelihood of developing schizophrenia. Studies have found that the death of the father before birth and environmental stress (Nazi invasion, natural disaster) both have an increasing effect on occurrence of schizophrenia. Unwantedness of the child by the mother, and depression during the last trimester also increased the risk for schizophrenia (3).
Rhesus incompatibility between the fetus and the mother (Rh-negative mother carrying an Rh-positive child) also increases the chances of developing schizophrenia. Rh incompatibility can also cause haemolytic disease and schizophrenia may be another effect of the disease (1). Birth complications can also be risk factors for the development of schizophrenia. Hypoxia (low oxygen levels during birth), low birth weight, central nervous system damage, and pre-eclampsia can also increase the risk for schizophrenia (2).
Although schizophrenia doesn’t manifest in its victims until early adulthood, prenatal and environmental factors have been shown to have a direct effect on the development of schizophrenia. Schizophrenia is still not understood very well, and until we understand the causation completely, we will never be able to successfully treat or prevent it. Schizophrenia is a devastating disease that affects all aspects of life. This intricate disease also brings up many questions regarding brain function. Why does it take over twenty years for this disease to come out? If the reasons for the disease have already developed, why does the disease lie dormant for years? If schizophrenia is due to brain damage from gestation or birth, why can people function normally for two decades before deteriorating? What exactly happens in the brain?
Works Cited
- Cannon, Mary., Jones, Peter B.., Murray, Robin M.., Susser, Ezra., Van Os, Jim. (Eds.) (2003). The Epidemiology of Schizophrenia. Cambridge: Cambridge University Press.
- Cannon, Tyrone D., Tiia Huttunen, Matti O. Huttunen, and Isabelle M. Rosso. "Obstetric Risk Factors for Early-Onset Schizophrenia in a Finnish Birth Cohort." The American Journal of Pscyhiatry 157 (2000): 801-808. Proquest. Bryn Mawr College, Bryn Mawr. 20 Feb. 2007.
- Faraone, Stephen V. & Tsuang, Ming T.. (1997). Schizophrenia: The Facts. (2nd Edition). Oxford: Oxford University Press.
- Opler, Mark G., and Ezra S. Susser. "Fetal Environment and Schizophrenia." Environmental Health Perspectives 113.9 (2005): 1239-1242. JStor. Bryn Mawr College, Bryn Mawr. 19 Feb. 2007.
- Torrey, E. Fuller. (2001). Surviving Schizophrenia—A Manual for Families, Comsumers and Providers. (4th Edition). New York, New York: Harper Collins Publishers.