Serendip is an independent site partnering with faculty at multiple colleges and universities around the world. Happy exploring!
Mental Health and the Brain: Tourette's, Migraine

|
Mental Health and the Brain:
|
|
Our ninth session and resulting on-line forum discussion started us on a discussion of particular instances of mental health issues in the context of our earlier discussions of the variety of available therapeutic procedures and of the brain. This week we move on from schizophrenia and depression to Tourette's syndrome and migraine.
Readings for this week
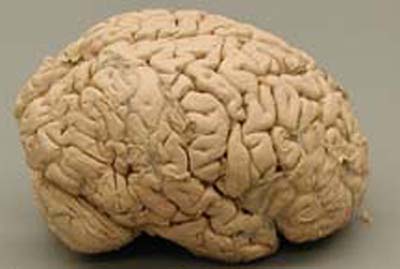
Tourette's Syndrome
- I have Tourette's but Tourette's doesn't have me
- The tics of Tourette's often go undiagnosed
- A surgeon's life (requires registration, also available here)
Relevant recent materials elsewhere
Where we've been ...
Depression is not an opportunity and it is not normal, it is not used to build character ... llamprou
"Pain hurts and it won't make you tougher" ... adiflesher, sam flesher
someone who has never even experienced depression can still sense its tremendous power, not only as a negative phenomenon, but in being able to yield something positive--like a new perspective on life ... dfeingold
I certainly believe that life is about encouraging an element of possibility and agency -- but I don't agree that helping to lessen severe suffering discourages that ... ysilverman
I see depression as an absolutely "normal" human occurence. And so, my next thought goes to...being with one's SELF and at the same time attached to another/ knowing how to be SELF without the other AND still attached ... merry2e
I understand the feeling that the "bad" things that happen to us help us grow, but at the same I know that some events in my life that have helped me become a more compassionate person I would still give a lot for them not to have happened ... Paige Safyer
This is a very sensitive topic and must be treated that way ... I think that saying that depression and schizophrenia (SZD) may have benefits implies that it's a worthwhile or valuable experience that everyone should have. Regardless of one's intention, I think this implication comes out (and I think this is why the conversation is so polarized) ... Paul B
for some people the proper approach is to relieve their suffering asap if possible, for others the only option might be to help them learn to live with it. For others it might be to allow them to suffer even though we could stop it because they are doing something with that situation which is valuable ... MartinBayer
"symptoms" whether a caffeine-induced headache, or a pervasive sense of sadness whose genesis is unknown can be a "signal" that there is something amiss... However, I don't know that the "symptoms" themselves are actually the problem, but rather a limited solution implemented by the storyteller that needs to be revisited. The symtoms, perhaps, are the "signal" that alerts us of the problem? ... Sophie F
one direction might be to continue to flesh out a more outside view of what depression really is ... perhaps
there is something wrong with the connections between the TK and the ST
(similar to Capgras). One line of information is coming in telling the
ST that someone just gave them a hug. However, the line that is
supposed to tell the ST that this is a pleasant experience and the
proper response would be to be happy or feel loved is malfunctioning
somehow. Second,
perhaps the malfunction is inside the ST. This seems like it would call
for a compartmentalization of the ST. We usually talk about it as a
black box. However, maybe there are pathways and connections within the
ST that are vulnerable to malfunction. For example, maybe all the
necessary ingredients have entered the ST via connections from the TK
and the "assembler," or the part that organizes them into a cohesive
story is malfunctioning. Or perhaps the "motivator," or the part that
sparks our motivation to construct a story in the first place is broken ... ryan g
I feel that this question of 'function' really deals with what we have been grappling with this semester and at the end of the day sums up how we could potentially change the mental health system. If we focus on the story teller then we are able to appreciate each individual experience for what it is and help every person reach a place where they can grow/learn/thrive to the best of their ability. If we focus on function, then we deal with external behaviours in order to make sure that individuals can experience a 'normative' reality ... How do we need to change to make that happen? ... akerle
A cure would not be aimed at changing the person itself, thereby eliminating a particular talent, but, on the contrary, at helping him/her flourish in all fields of his/her social life ... vpizzini
Therapy, drugs, just sitting around and thinking – all of these are ways to change brain chemistry, why are some more “natural” than others? ... kmanning
Being stuck and feeling like one cannot emerge from the tangle of one’s mind seems a common experience to both [depression and schizophrenia] and one that is not trivial ... Sophie F
not all psychologists believe in agency. Stunningly most don't. I emphatically do. .... I had a frontal lobe tumor and frontal lobe syndrome ... schizophenia is also a disorder of free will. .... "Someone is controlling my thoughts" That is a common delusion. In my considered clinical judgement restoring that agency is a prime objective. Without that, life is not much fun and the stories you tell tend to be kind either very dull or really terrifying. Both somatic and talk therapies ought to take that as a first target ... Sam FlesherTake off points - Tourette's
Diagnostic Criteria for 307.23 Tourette's Disorder;
- both multiple motor tics and one or more vocal tics must be present at the same time, although not necessarily concurrently;
- the tics must occur many times a day (usually in bouts) nearly every day or intermittently over more than 1 year, during which time there must not have been a tic-free period of more than 3 consecutive months;
- the age at onset must be less than 18 years;
- the disturbance must not be due to the direct physiological effects of a substance (e.g. stimulants) or a general medical condition (e.g. Huntington's disease or postviral encephalitis)
Oliver Sachs ...
"Then Bennett took the knife, made a bold clear incision-there was no hint of any ticcing or distraction-and moved straightaway into the rhythm of the operation. Twenty minutes passed, fifty, seventy, a hundred. The operation was often complex-vessels to be tied, nerves to be found-but the action was confident, smooth, moving forward at its own pace, with never the slightest hint of Tourette's...Here, then, was an entire operation without a trace of Tourette's. Not because it had been suppressed, or held in-there was never any sign of control or constraint-but because, simply, there was never any impulse to tic."
"What most of us call a startling or "abnormal" speed of movement appears perfectly normal to Touretters when they show it This was very clear in a recent experiment of target pointing with Shane F., an artist with Tourette's. Shane showed markedly reduced reaction times, reaching rates of almost six times normal, combined with great smoothness and accuracy of movement and aim. Such speeds were achieved quite effortlessly and naturally; normal subjects, by contrast, could achieve them, if at all, only by violent effort and with obvious compromise of accuracy and control."
"The real problems, the inner problems, are panic and rage-feelings so violent that they threaten to overwhelm him, and so sudden that he has virtually no warning of their onset...the strain of controlling himself is severe and exhausting"
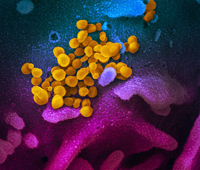
Take off points - migraine
From David W. Dodick and J. Jay Gargus, “Why Migraines Strike” Scientific American, July 2008
"In addition, the activity of these cells [three clusters of cells in the brain stem—the locus coerulus, raphe nucleus, and periaquedcutal gray] is modulated by the behavioral and emotional state of the individual—factors that can trigger migraines. These brain stem areas receive input from only two areas of the cortex, the limbic and paralimbic cortices, regions that regulate arousal, attention and mood. Through its connection with the brain stem, the limbic cortex affects the functioning of the rest of the cortex—a fact that might explain how emotional and psychological stress could catalyze migraines, why mood fluctuates during migraine, and why there is an association between migraine and depression and anxiety disorders, both of which occur more commonly in migraine sufferers than in others."
From Jeff Tweedy, “Boy Meets Pain”
"When I was growing up I lived in a household with caring people — my parents were definitely nurturing and wanted me to be happy and healthy. But it was a different time. If a kid was suffering from a mood disorder in my parent’s generation, the typical response was likely to be, “What are you crying about? I’ll give you something to cry about.” That sounds really harsh but it’s a reality of my childhood. It was much more difficult for me to explain, “I just feel sad for no reason,” than for them to see I was in literal pain. So I think there’s some connection there. In other words, the psychological suffering of the mood disorder may have manifested itself in a very real pain of the migraine that was much easier to express. It’s obvious your kid is hurting when he can’t stop vomiting and he can hardly open his eyes. And with my mother having migraines herself, she could identify – she knew they were real. There’s a lot to explore there — there was for me — how much of it was an outward manifestation of a mood disorder.
…
I’ve noticed that the arc of a migraine is very similar to some of the traits of panic disorder.
One of the things that happens a lot with panic disorder is that you’ll have an actual panic attack and for weeks or months after that you’ll have a fear of a panic attack that can heighten your anxiety and heighten your stress levels to the point where you end up having another panic attack. To me those things mirror each other. Migraines would add stress to my life in a way that would contribute to the next headache and it would begin a cycle that would be hard to stop. So I would have periods where I would have a migraine very frequently — every other day or twice a week — for months.
The hospital I went to in 2004 to address my painkiller addiction (which happened in part due to the migraines) was a “dual-diagnosis” facility — they treated my panic disorder and depression simultaneously. And I found that once I was able to manage those two things, I’ve been able to be mostly migraine-free for the last four years. For me, that solidified my theory about the connection.
From “Less than you Think” by Jeff Tweedy, Wilco
Your mind's a machine
It's deadly and dull
It's never been still and its will
Has never been free
Lightly tapping
A high-pitched drum
As your spine starts to shine
You shiver at your soul
A fist so clear and climbing
Punches a hole
In the sky
So you can see
For yourself
If you don't believe me
There's so much less
To this than you think
From “Arms at Rest” by Siri Hustvedt
"As a child, life with my peers in school was always hard for me, and my yearly purges [associated with migraine] no doubt served a purpose. For two days a year, I suffered a cathartic dissolution, during which I was able to stay home and be close to my mother. But times of great happiness can also send me over the edge — the adventure in Thailand and falling in love and getting married. Both were followed by a collapse into pain, as if joy had strained my body to its breaking point. The migraine then became self-perpetuating. I am convinced that a state of fear, anxiety, and a continual readiness to do combat with the monster headache pushed my central nervous system into a state of continual alarm, which could only be stopped by a deep rest. I continue to cycle. Periods of obsessive and highly productive writing and reading that give me immense pleasure are often followed by a neurological crash — a headache. My swings from high to low resemble the rhythms of manic-depression or bipolar disorder, except that I fall into migraine, not depression, and my manias are less extreme than those of people who suffer from the psychiatric illness."
From “In Bed” by Joan Didion
"But not all perfectionists have migraine, and not all migrainous people have migraine personalities. We do not escape heredity. I have tried in most of the available ways to escape my own migrainous heredity (at one point I learned to give myself two daily injections of histamine with a hypodermic needle, even though the needles so frightened me that I had to close my eyes when I did it), but I still have migraine. And I have learned now to live with it, learned when to expect it, how to outwit it, even how to regard it, when it does come, as more friend than lodger. We have reached a certain understanding, my migraine and I. It never comes when I am in real trouble. Tell me that my house is burned down, my husband has left me, that there is gunfighting in the streets and panic in the banks, and I will not respond by getting a headache. It comes instead when I am fighting not an open but a guerilla war with my own life, during weeks of small household confusions, lost laundry, unhappy help, canceled appointments, on days when the telephone rings too much and I get not work done and the wind is coming up. On days like that my friend comes uninvited.
And once it does, now that I am wise in its ways, I no longer fight it. I lie down and let it happen. At first every small apprehension is magnified, every anxiety a pounding terror. Then the pain comes, and I concentrate only on that. Right there is the usefulness of migraine, there in that imposed yoga, the concentration on the pain. For when the pain recedes, ten or twelve hours later, everything goes with it, all the hidden resentments, all the vain anxieties. The migraine has acted as a circuit breaker, and the fuses have emerged intact. There is a pleasant convalescent euphoria. I open the windows and feel the air, eat gratefully, sleep well. I notice the particular nature of a flower in a glass on the stair landing. I count my blessings.
From Oliver Sacks, Migraine
Case 68: This 32-year-old man was an ambitious and creative mathematician whose life was geared to a weekly psychophysiological cycle. Towards the end of the working week, he would become fretful, irritable and distractible, “useless” at anything save the simplest routine tasks. He would have difficulty sleeping on Friday nights, and on Saturdays would be unbearable. On Sunday mornings he would awaken with a violent migraine, and would be forced to remain in bed for the greater part of the day. Towards evening he would break out in a gentle sweat and pass many pints of pale urine. The fury of his sufferings would melt away with the passage of these secretions. Following the attack he would feel a profound refreshment, a tranquility, and a surge of creative energy which would carry him to the middle of the following week. (page 68)
…
“’Economic” considerations were also forced on my attention by another patient, the migrainous mathematician, who was among the first I saw. With this patient, to continue the history, it was easy to find antimigraine drugs. Ergot worked, and worked very well; but when I cured him of his migraines, I cured him of his mathematics too—he seemed, however paradoxically, to need one for the other. At this point, he said, “I’ll keep my migraines—I think we better keep everything as it is.” This experience also served to reduce my own impatient need to “treat,” and disposed me to listen more carefully to the patients, to that whole pattern of “ever-changing features and factors which the migraine patient both suffers and creates.”
Such considerations do not arise, or arise less, when migraine is occasional—when attacks come, for example, once a month or less. But if migraine is severe, if it intrudes more into life, then complex interactions are bound to occur, and treatment should not be “purely physiological.” One would not, of course, deny physiological treatment—one would seek out whatever drugs, or other measures, to help the patient. But, at the same time, one should search more deeply, both patient and physician should search more deeply; for migraine, when frequent, is not just a disease, but a whole way of being, which forces the organism into special adaptations and identities. (page 268)
...
Case 81
This 55-year old man had been a former inmate of Auschwitz. He had suffered about one attack of classical migraine a month from the age of 7 until his incarceration in Auschwitz. During his 6 years in the concentration camp—6 years during which his wife, parents, and all other close relatives were killed—he did not experience a single attack of migraine. He was “liberated” by the Allies in 1945, and the following year emigrated to the U.S.
Since that time, he has been chronically depressed, guilt-ridden, preoccupied with the deaths of all his relatives, whom he feels he might have saved, and intermittently psychotic. During this time he has also experienced 6 to 10 attacks of classical migraine each month, attacks which are refractory to treatment, an accompanied by the intensest suffering.
He is also considerably “accident prone,” and during the two years that I saw him managed to sustain a Coles fracture, a fracture-dislocation of one ankle, and a head-injury. Each of these injuries was followed by several weeks’ remission of his migraines. It is also fo interest that on the three occasions in which he has been hospitalized for psychotic depression during the past 20 years, he was free from migraines. (pg. 168-69)
From Freud: “…Although it may be said…that he has taken “flight into illness,” it must be admitted that in many cases the flight is fully justified, and the physician who has perceived this state will silently and considerably retire…Whenever…advantage through illness is at all pronounced, and no substitute for it can be found in reality, you need not look forward very hopefully to influencing the neurosis through your therapy.” (qtd. in Sacks, Migraine, page 237)
And a final word from Sacks: But a migraine patient is not just complaining of a recurrent dysfunction—he is telling us, if we will listen, the story of his life, or patterns of living, and patterns of reacting, and (perhaps) deep patterns of which he has no conscious awareness, any of all of which may be relevant to his migraines. We cannot know in advance, on first meeting him, what is relevant or irrelevant. It is crucial to enquire minutely into all the circumstances of attacks—when they are most common, when they are rarest, what are their patterns and provocative triggers. But at a deeper level, one needs to know the “economy” of a life, the psychological and physiological “needs” of an individual. And this is not something which can be ascertained in a quick or casual way—it requires a relations between patient and doctor, and an insight, on the sufferer’s part, not to be achieved in a moment, as to the connections between the patterns of his life and his migraines. It requires, to some extent, making the unconscious conscious or, in Freud’s words, replacing an “It” with an “I.” (page 267)


Comments
"Tea kettle reality" is
"Tea kettle reality" is elusive not illusive.
Our discussion of mental health seems plagued by words like comfortable, acceptable, or fitting in. This kind of language reeks of mediocrity when health is about excellence. When we talk about physical health we think of toned muscles and strong backs, not your average joe-six-pack who just "fits in".
When we speak of a spectrum of illness, any kind of illness, we are still talking about something which is categorically different from health. Certainly each individual experiences a variety of aspects of healthfulness, both mental and physical, but that does not mean that health and unhealth are merely quantitatively different; they are in fact qualitatively different. If I have a cut on my arm I would say that my arm is injured/has a problem that needs fixing. But, a cut lies on the spectrum of illness that does not require intervention... most of the time. Likewise with mental illness I think that we can say that many mental health issues lie an a region of the spectrum of problems/ilnness that does not require intervention. But to say that the cut is "not a problem" or that even mild forms of mental illness are "not problems" is... I can't think of a better way to say it than to say it... is wrong.
I think it is far more realistic to try to dry lines between qualitatively different things than it is to draw them between quantitatively different things. Ryan's discomfort with drawing a line is totally legitimate because thus far our conversation has considered all mental states as qualitatively the same.
Other than this point I am in total agreement with Grob's 7 points.
Don't get me wrong, I am all for diversity. I don't want everyone to think, talk, act, and look just like me but, for their own benefit, I do want everyone to live in the "tea kettle" reality which is dictated not by any culture but by the laws of nature (gravity pulls things down type laws).
In regards to the "moral comfort blanket". I think that it is dangerous to think like that because you will set up default "protocols" for action which may not be applicable to particular circumstances. Each situation should be examined individually. To think one has a set of rules/safety blanket to guide them through every decision will cause problems.
continuation of the tea kettle story
I offer this story in addition to the story I shared in class about the schizophrenic and the tea kettle. A woman is experiencing a period of intense grieving after the loss of her husband. She sets a tea kettle on the stove and sinks into a series of sad memories about her loved one. In a distracted daze, she decides to take a bath to sooth herself, forgetting about the tea kettle… This was an isolated incident.
A last statement about the logistics of the tea kettle problem, it is only after frequently repeated activations of a smoke detector that the fire department will fine and further more jail an offender. A little sensitivity to accidents, behavior modification, and story revision here?
I wouldn’t argue that an aim of any mental illness treatment must involve teaching the patient tea making techniques. In fact, I have been pondering ways of separating the tea kettle problem from the concept of being out of touch with reality. What I would like to say is that maybe the therapist can help the patient reflect on their behaviors and the underlying story. Therapy should be about creating a coherent story oneself, including interpersonal and environmental interaction. If one has the intention to make a cup of tea, some part of the mind should track the progress toward realization of that goal. The person should at some point realize that they have not completed the task.
Memory plays an important role here. I am uncertain about whether this is the responsibility of the storyteller or the unconscious. Certainly, the unconscious is capable of performing actions without storyteller involvement, like sleepwalking. So maybe the storyteller was never involved? Does the storyteller ever participate in tea making? The role of the storyteller is to integrate unconscious activity into a coherent story. So there is some minimal requirement for storyteller involvement here.
Tangles
Something that has emerged for me over this semester is the sense that mental illness, yes, exists along a continuum, but that depression and schizophrenia in two different people with equal “capacity” to participate in life are really quite similar. That is to say, that it’s all kind of the same. I understand that individual experiences are different, but they are anyway, given that reality is itself illusory in the sense of one “reality.” The task of coming to grips with what is “mental health” seems less daunting when seen along a continuum, Tourette’s syndrome, migraine, depression and schizophrenia are all attempts by the storyteller to reconcile information from tacit knowledge and sensory information. If this is so, perhaps not exactly as I’ve described it, but to the extent that the similarities exist more than we currently acknowledge, there is so much hope for a more holistic approach to mental health, one that nurtures individual strengths and does not fault people for non-normative behavior that is not dangerous. I think taking normative measures as a goal of mental health treatment is a potentially dangerous undertaking. As I’ve mentioned before, I think the more we shape peoples’ behavior to a “norm” the more we narrow the range of acceptable behaviors and the more alienated and disenfranchised those who do not fit the mold, in one way or another, are likely to feel. Besides life is more interesting in color than in black and white alone. The very goal of “fitting in” is a cultural one, I think. In cultures where there is greater acceptance of a variety of behaviors, a variety of mental states, as we know them, “fitting in” is likely not even a part of the calculus.
In thinking about migraine, Didion’s reference to migraine as “friend” intrigued me. We are so prone to seeing pain, illness (mental and physical) as enemy that perhaps we miss the parts of these experiences that can be useful. I know Lisa disagrees with me on this, so please fire away! This is not meant to trivialize the anguish, disconnectedness, discomfort, etc. of mental illness, but there is something to be said, in certain instances, for seeing pain as a means to an end. For if it is, in the most literal sense, a way for the mind to reconcile conflicting signals than it may not be foe at all, rather a remarkably resilient and resourceful, albeit imperfect, system for creating meaning out of disparate bits of information, many, many disparate bits of information, making the entire system so very remarkable, despite its imperfections. Just because I think pain is a signal from the body (the mind) that something is amiss, I would never wish a mental illness upon anyone, just as I wouldn't wish diabetes or a dislocated shoulder on anyone. However, if dis-ease is a signal to reevalute one's course, our brain's are shouting at us that we need to re-learn something. So, yes, crafting a new story, making new meaning and responding to the distress signals of our bodies are de facto "learning." Whether one sees that as "good," "bad, " "necessary" or something else is another matter entirely.
Should a migraine strike, it’s doubtful I’ll utter the phrase, “Welcome back, friend.” However, it may in fact serve one not to fight pain, or illness, but to come to terms with it in a meaningful way, meaningful for the individual, not by an outside standard. And, in this sense, medication alone as an antidote may not be the best long-term, expansive treatment for mental illness. Creating new meaning from existing stories is not something that comes "naturally" or "easily" to people with various mental illnesses, so if the goal is to create a story that uses the same information, but crafts a story that enables an individual to reach her potential (yes, a vague and indefinable entity, but nonetheless, a "real" one) than mental "health" has been achieved. Mental health is a journey, not an endpoint alone. I'll never be an olympic athlete, but I can certainly train to be in better condition than I am (perhaps, my laziness cannot be "cured").
mental health: more coherent directions?
Some further thoughts along these lines, stemming from our discussion last week having to do with "normative reality," "the world is social," and we are a part of the environment people need (want?) to adapt to ...
Do people "need" to adapt to particular "social" worlds? Is it the business of mental health to help/encourage them to do so? There are lots of pretty horrendous examples of problems with this approach, not only in other countries (psychiatric institutionalization in the USSR, for example) but in the US as well (homosexuality, lobotomies, ambiguous sexuality, to mention a few). I, for one, am less comfortable with a mental health approach that uses the ability to deal with "normative" reality" (or "tea kettle" reality) as a goal and more comfortable with one that uses, instead, enhancing the ability of individuals to conceive and revise their own individual stories. This leaves room not only for acknowledging "neurodiversity and its value," but, more explicitly, for including within the mandate for mental health professionals changes not only in individuals but also in cultures. My guess is that more attention needs to be paid not ony to the role of stories in mental health issues but also, in particular, to the problem of conflicts between individual and social/cultural stories, and our tendency to automatically give priority to the latter.
And some further thoughts about more general patterns coming from thinking about depression and schioprenia, together with Tourette's and migraine. One sees, in all four cases
- a continuum from "normal" to troubling
- some positives as well as some negatives
- a complex mix of genetic/environmental/cultural influences
- a research trajectory implying an absence of not only simple causes but also simple cures
- a social/cultural impatience with problems lacking simple causes/cures, and people who present them
- the possibility that troubling "symptoms" are at least to some extent an effort on the brain's part to find an adaptive way to cope with problems, often with a significant story telling element
- in the most troubling manifestations, a commonality of feeling an inability to control one or another aspect of oneself
Maybe this usefully points a useful direction for overcoming some of the troubling fragmentation of current approaches to mental health? Perhaps there actually is some commonality to what otherwise might appear to be a diverse array of independent problems in this realm? And some progress might be made by recognizing such commonalities and using them as a foundation for developing new directions in therapeutic practice, in research agendas, and in social/political policy?I am not a fan of a
I am not a fan of a normative view of mental health either. There are too many issues with where to draw the lines. I would tend to lean towards a more individualized model of a mental health goal. Whether that be fulfilling potential, creating meaning or whatever. That being said, I haven't necessarily found one that stands out in my mind as rock solid. So, to answer the question of whether it is the business of mental health providers to encourage/help people fit into a normative society. I would say no... unless they want help fitting into that society.
As an aspiring physician, I have been kicking this around in my head a bit. What is the role of the health care provider? When do they step in? What authority do they have to tell someone they should be this or that? It seems to me that if in general you adopt the principle that you are going to help the individuals who want help to achieve their goals (fitting in to society, freedom from suffering, losing weight, better vision etc. ) and you do this to the best of your ability using the tools you have available, then you are fulfilling your purpose as a health care provider.
Anyway, that is my current solution for cocooning myself up in a blanket of moral safety as I head into healthcare. However, I realize that the "only help those who want help" model of mental health care has some serious shortcomings. For example, what to do about those individuals who can't really say whether they want help or not. I'm still working on it... I'll keep you posted.
holes in moral safety blankets?
It seems to be that both of
It seems to be that both of these ideas can be addressed if we look at the job of a mental health worker not as a vehicle to get people where they want to go, but rather to help bring them to a place in which they feel comfortable existing. Often times people go into therapy with specific concerns about life, relationships, problems, etc. and yet, don't come out a successful therapeutic experience with those issues solved -- instead, if things have worked, they have been resolved. I think that this is why, specifically, I felt something was remiss with CBT, as what we think we want to change is often not what ends up needing changing. I think a goal of fitting in or acclimating may not mean changing oneself as much as it means changing how one views oneself in the scheme of things, changing how one wants to be viewed, changing how one views other people. If I feel I fit in, then I do, don't I? (It's not as if it is a card-carrying club.) And, in that direction, I think helping someone "fit in" is exactly what therapy is always for -- leading someone to the life they want to be leading.
I also am interested in the issue Ryan raises. What about someone with schizoid personality disorder, with no interest in social relationships, and very little ability to experience pleasure? Often this person won't present for treatment. Often they won't even feel dissatisfied with their status quoe. But is there room for a mental health professional to say, wait, there is a potential problem here?
Post new comment