Serendip is an independent site partnering with faculty at multiple colleges and universities around the world. Happy exploring!
On Infections and Inequalities: The Modern Plagues, by Dr. Paul Farmer
We don’t have to be expert in foreign affairs to have an opinion as to how much security the industrialized nations of the world brought with the $300 million they spent over ten years to eradicate smallpox, as compared to what was achieved with the $28 billion spent in 1983 alone for arms exports to Third World countries. Perhaps a few million dollars given to improve the health of the children of Central America would bring more security t o the area than the billions we have spent to arm the parents—and often the children.
-Howard Hiatt, 1987
Paul Farmer has been one of my idols and heroes since I first read Tracy Kidder’s Mountains Beyond Mountains: The Quest of Dr. Paul Farmer, A Man Who Would Cure The World. I have since read several of his books, now including this one, seen him speak and even met with him. Infections and Inequalities deals with Farmer’s fundamental theory: that “cost-effective” healthcare, that is, denying the world’s poor expensive treatment and focusing on preventative medicine, is no way to treat a patient, however poor they may be. Farmer argues, and I agree, that we need to eradicate this notion of “cost-effectiveness” and create solutions that enable us to bring both preventative and restorative medicine to the developing world. While malaria nets and preventative medicine and education are part of the puzzle, heart surgeries and AIDS drugs also need to be made available to the world’s poor. “Nothing is wrong with high-tech medicine, except that there isn’t enough of it to go around. It is, in fact, concentrated in precisely those areas where it will have the most limited effects. We need more and better service for those marginalized by poverty and by discrimination”2 (14). Preventative medicine has long been seen as the most cost-effective and reasonable way to deal with healthcare in developing countries. Economically speaking, preventative care seems to make sense—there isn’t a lot of money for healthcare, and it is more efficiently used to buy mosquito nets for a million families rather than to buy heart surgery for one little boy. To ask for one such surgery in the face of such devastation would seem ludicrous. And yet, as Farmer aptly questions, “[don’t] the dilemmas of the [world’s] sick call for a full range of high-tech and low-tech interventions? Why….[is] it so manifestly impolitic…to press for the former as well as the latter?”2 (21) In one of his first projects, establishing a hospital on Haiti’s Central Plateau, Farmer works with a priest who brings him to the site of the first latrines ever built in the village. They are cement, the most solidly built structures in the entire place, and Farmer questions whether they are “really ‘appropriate technology’ for such a poor village. The priest [is] furious. ‘Do you know what “appropriate technology” means?’ he finally answer[s]. ‘It means good things for rich people and shit for the poor’”2 (21). Too often in healthcare, especially in the United States, we are forced to choose between extremes—expensive, state-of-the-art treatment—or nothing at all. And those who can afford the costliest medicine also tend to be the healthiest due to their living situations, while the poor are susceptible to more diseases in cramped, unsanitary living environments and forced to accept inadequate medicine. If we continue to push only for preventative medicine, clinics, and dispensaries in developing countries rather than real hospitals and proper care, the world’s poor will never win.
We know most things about it, but TB still kills more people than any other pathogen, far more than alcoholism, AIDS, malaria, tropical diseases and Ebola combined, and nobody seems to care…Where is the shame? Where is the outrage?
-Lee Reichman, 1999
Infectious disease is fascinating (and infuriating) not only from a biological standpoint, but also from a social one. Tuberculosis, for instance, a virus which hasn’t really been seen in the US for decades, will infect 9 million people globally and kill 4 people a minute, about 2 million people (almost all in the developing world) this year1. This inequity of such a disease is largely due to what Farmer aptly characterizes as the “semi permeable membranes, often quite open to diseases and yet closed to the free movement of cures”2(55) that are political boundaries. A disease which calls for aggressive treatment in Texas or New York may be left undiagnosed and fatal in Mexico and South America. Though our health care system in the United States is far from perfect, we have the resources at our fingertips to fight infectious disease. Why should these resources be confined to the places that need them least? In general, the US is already less susceptible to such diseases simply because of its higher standard of living, and yet we make the cost of the drugs to fight such disease so high it is impossible for those who need them most to acquire them. “’Medicine [has become] big business,’ observes one report. ‘Patients turned into profit centers; their many ailments, product lines’”2(279).
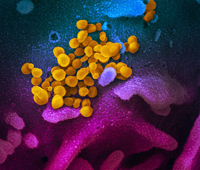
Also known as the “Wasting Disease” (for the way it destroys victims physical capabilities) and the “White Plague” (for the pallid color of a patient’s skin), TB is a communicable disease caused by the bacteria Mycobacterium Tuberculosis. The bacteria, called bacilli, settle in the lungs and lymph nodes of a patient, where they are protected by a thick coat of wax that enables them to cling to the walls of the lungs and lie dormant for years. This inactive state of the bacilli is called “Latent TB Infection” (LTBI) and is asymptomatic, though it may result in the bacteria spreading to other parts of the body such as the kidney, spine, or brain, where it is not contagious and is normally mild. In 1-5% of patients, this Latent TB morphs rapidly into TB disease (Primary TB), while in others (5-9%) active TB may develop many years after infection (Post-Primary TB, Secondary TB, Reactivation TB disease). When the immune system of a person with Latent TB is weakened or compromised the bacteria become active and progress into “Pulmonary TB”, a disease of the lungs. Symptoms of Pulmonary TB include a persistent cough that lasts for over several weeks, weight loss, loss of appetite, high fever, night sweats, and violently coughing up blood. A person with Active TB can infect up to 20 people a year through simply coughing, sneezing, speaking, or spitting—meaning that even health care workers and doctors treating the disease are at a very high risk of contracting it themselves, especially in poor countries where medical facilities are unclean or crowded. In only about 10% of those who become infected by the bacilli and have a healthy immune system does the infection become the disease; however, it continues to kill millions each year.
Active Pulmonary TB, without the proper treatment, kills over 50% of patients who develop it. Though this mortality rate is comparable to that of the Black Plague and the Avian Bird Flu Pandemic, Tuberculosis—a disease spread simply by talking and sneezing—is rarely thought of by Americans as a threat. This is mostly because it isn’t a threat—at least in our safe, comfortable world of affordable treatment and early detection. For those living in poverty, however, it continues to be one of the deadliest diseases in existence—spread quickly and easily, with its only cure being extensive, costly treatment, it is a disease that warrants everyone’s attention, not only of those whom it currently affects.
One of the greatest perils of ignoring infectious disease in underdeveloped countries is that of the emergence of drug-resistant strains. As Tuberculosis is left untreated or partially treated, it morphs into what is known as “MDR-TB,” or Multi-Drug Resistant Tuberculosis. “In failing to prevent or contain resistance to first-line drugs, ‘we are unwittingly transforming an eminently treatable infection into a life-threatening disease that is exorbitantly expensive to treat” (273). This can happen for many diseases—if drugs and antibiotics are administered incorrectly or not at all, viruses, which are highly adaptable organisms, modify themselves to overcome the initial treatment regime and are no longer responsive to the first line drugs used to treat them. MDR-TB is spread just as easily as regular Tuberculosis, and yet is far deadlier and the drugs needed to treat it far more expensive. And because TB drugs require such regimented treatment, often necessitating that patients travel to the clinic on a regular basis for administration, it can be difficult to ensure that they are habitually taking their medications. Tuberculosis treatment lasts anywhere from 6-9 months, and yet, patients often feel improvement before then and discontinue taking their medications, which can lead to the development of MDR-TB. Though it is currently treatable, it has mortality rates comparable to those of regular TB before antibiotics were developed and is over one hundred times more expensive and difficult to treat, requiring up to two years of intensive chemotherapy that wreaks havoc on a patient’s immune system. This drug resistant strain crushed the hope that TB would be eradicated within the near future and generated a greater threat—that the disease, if not treated properly, will evolve into an untreatable, swiftly spreading pandemic. Indeed, just this past year a new strain of TB, called XDRTB—Extensively Drug-Resistant Tuberculosis—has in appeared Europe, Asia, Africa, and North and South America. This strain is resistant to the line of drugs used to treat MDRTB, and is virtually untreatable. To avoid the complete morphing of TB, countries and their governments must provide necessary funding and instigate the DOTS strategy put forth by WHO in 1991. Leaving TB untreated or undetected needlessly wastes millions of lives each year and could have disastrous consequences for the entire world.
Farmer makes an interesting point throughout his work that reminds me of a class discussion we had early on in the semester and an idea that has been raised several times since then. It parallels the “nature vs. nurture, genes vs. environment” controversy, in a way. Farmer explains that “To understand these realities [the social realities that exacerbate infectious disease], nothing less than a biosocial analysis will do—an analysis that draws freely on clinical medicine and on social theory, linking molecular epidemiology to history, ethnography, and political economy”2 (5). Everything is interdependent. Just as we depend on the “water wheels” of the sun and the breakdown of energy, infectious diseases depend on biological cases that arise from the water wheels of social structures and economical inequalities. “Thus do fundamentally social forces and processes come to be embodied as biological events” 2 (14). It is an interminable cycle: povertyàpoor health careàlower productivityàpoverty. This means that TB and other infectious diseases, such as malaria, need to be examined and treated not only in the realm of medicine and biology, but also addressed in the social realm.
What the social world has made, the social world, armed with knowledge, can undo.
-Pierre Bourdieu, 1993
As our world becomes ever more universal, so do our problems, both our social diseases and our biological ones. Travel and technology have made the world more accessible than ever before, and yet they have also brought new realms of inequality, both in medicine and economics, across our borders. For us to continue living in such an international society, we must examine the impact of our policies on the health of the global world—not only economically, but in the medical and social realms as well. What we desire for our children let us desire for the children across the borders as well—quality healthcare, good jobs, livable wages, and the right to be free from curable infectious disease.
Bibliography:
1 Running Out of Breath: TB Care in the 21st Centur, Doctors Without Borders, http://www.doctorswithoutborders.org/publications/reports/2005/tbreport_2005.pdf
2 Farmer, Paul. Infections and Inequalities: The Modern Plagues, Berkley: University of California Press, 1999.
3XDRTB, http://www.greypath.com/node/5532
4WHO: The Stop TB Initiative, http://www.who.int/tb/features_archive/stop_tb_strategy/en/
5 Medline Plus: TB, http://www.nlm.nih.gov/medlineplus/tuberculosis.html
6 The Global Fund, http://www.theglobalfund.org/en/


Comments
medicine and public health
Uh, In your infectious disease section you refer to tuberculosis as a virus. It is a bacterium. You may find my health oriented essays of some interest.
Even so, the body of your work is sound, and persuasive, written to good effect.