Serendip is an independent site partnering with faculty at multiple colleges and universities around the world. Happy exploring!
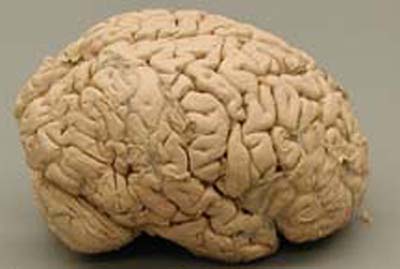
Mental Health and the Brain: Talk Therapies

|
Mental Health and the Brain:
|
|
Our eighth session and resulting on-line forum discussion considered pharmacotherapy and experiential therapy in the context of our earlier discussions of the brain. This week, we will continue our discussion of pharmacotherapy and move on to begin to think about additional forms of talk therapy in the context of earlier discussions of the brain.
Readings for this week
Psychoanalysis
- What is psychoanalysis?
- Dream interpretation and psychoanalysis
- Psychoanalysis then and now
- Freud is widely taught at universities, except in the psychology department
- A new and controversial short term psychotherapy
- Psychoanalytic therapy wins backing
- Have you ever been in psychotherapy, doctor?
Cognitive behavioral therapy
- Making sense of cognitive behavioral therapy
- Changing politicians' minds about changing our minds?
- Dodo bird, phoenix, or urban legend? The question of psychotherapy equvalence
- Like drugs, talk therapy can change brain chemistry
Where we've been ...
forms of talk therapy (with a medical professional) that are used as a continuous crutch for people throughout life is an unneccessary strain upon an already strained healthcare system. I think the type of support that people get via talk therapy when they don't really have an underlying problem can and should be found among friends and family ...For that reason I instinctively dislike activities like the one we all participated in last monday. I think they can be breading gounds for peoples desire to seek self affirmation when what they might need is a stern but caring friend/realitve to tell them to cut the crap and do x y or z ... MartinBayer
people in today’s society have begun to depend upon talk therapy so completely that often times they are no longer capable of thinking about issues and problems by themselves and coming to productive and coherent solutions ... llamprou
we aren't as clueless to the machinations of our mind as we sometimes imagine/present ourselves to be. But I think a lot of times we are clueless as to how we can exact change, and that is where professional help can be of use to most people ... ysilverman
I thought the talk therapy activity was interesting and difficult. I like being given ample time to consider different situations, especially when people are involved. I find that .... when put in groups ... I go blank. I don't like saying things that don't have some sort of conscious foundation in my head in front of a group of people, since I like to be able to expand on and defend my views .... I think it's also hard to genuinely tell someone you barely know why you think you can relate them to others in your life ... kgins
I really enjoyed the exercise we did in class with Sarah. For me, it was a novel way to enact the working of tacit knowledge. Prior to the exercise, I did not have a working knowledge that I may have certain intution about people. The exercise brought to light some of those unconscious understandings and crafting a story after being drawn to a particular person pushed me to examine and understand my intuition in a way that I likely would not have done otherwise ... I think a general sense of interpersonal disconnection is very much a theme of modernity. As such, therapy can enable an interpersonal connection that people may not be encouraged to foster in daily life ... Sophie F
So, one of my issues with therapy is... how does it work? What is
the mechanism? I am not arguing that talking, or culture, can't affect
our brains. I'm just saying that if most or all of us exists in the
neural circuitry of our brain, then why don't we focus on manipulating
that circuitry to achieve the changes we want? ... This is why
drugs are particularly interesting to me right now. They seem to
provide a concrete way of providing change. This also seems to be why
drugs have more credibility than therapy too. Some guy in a white coat
can stand up there and say "Pill X affects structure Y which is
responsible for symptom Z." ...
I'm not saying that therapy doesn't work. I'm sure it does for some
people... maybe it could for all people. I think we can accept that
and move on. I think a more useful question is how does it work? How does it change the neural connections that shape my experience. I
feel like the answer to this question, as well as a more subtle
understanding of the connections in the brain and our ability to
manipulate them will lead to the next generation of treatment ... ryan g
The more I learn about the physiological effects of talk therapy, the more I find it hard to talk in terms of the story teller, because it seems to be glossing over, as Ryan mentioned, the physical mechanisms in the brain for how it works. We know the story teller does effect changes in brain chemistry that can be measured through scientific tests, and I feel like this should prove once and for all that talk therapy and drugs are working towards the same goal ... kmanning
To really define mental health and mental illness - I think we have to continue talking about the storyteller even in cases like my father's where the root cause of the illness could be clearly traced to a very clearly identified problem with a brain structure ... adiflesher
Throughout last class, I was thinking that perhaps the storyteller is responsible for depression, bipolar, etc ... I think a faulty storyteller can tell a story that is far from reality and lead to bad thoughts ... I think the drugs are effective in that they predispose one to more pleasant thoughts and make people receptive to therapy. However, I believe that it is only through therapy that one can adjust their storyteller to tell stories that are more in touch with reality ... Paul B
I understand talk therapy to work as a series of inputs to the brain,
via the usual physical structures. These inputs are interpreted by the
cognitive unconscious and the storyteller. What is special about these
inputs is that they are designed to target storytelling activity and
inspire introspection and revision. Perhaps by altering the existing
neural circuitry ... jrlewis
Take off points - psychoanalysis, dynamic psychotherapy
Dynamic Psychotherapy is basically the same process except much faster and more directed.''When the patient comes,'' he said, ''immediately I am focusing on the patient's feelings. I am constantly, actively involved.'' Thus he altered free association, Freud's passive technique of letting the patient lie down and talk about whatever comes to mind, and replaced it with ''focused free association.'' Free association plodded an unnecessarily circuitous route through the psyche, he thought. You couldn't tell where it would take you or for how long. There were no existing studies regarding its effectiveness - and it seemed that there never would be any.
He (the therapist) forces the patients to plumb the source of their problem behavior in 15 to 40 sessions, rather than waiting until the patients are ''ready'' to bring up painful experiences. The therapist actually badgers them into discussing these episodes, refusing to let the patients shy away from discussion or cover up their emotions.
A new and controversial short term therapy
Psychoanalysis is unscientific. Its theories and assumptions are not based on observation or experiment. It is an impediment to progress in social science and it is a social nuisance, and society would be better off without its bizarre armchair fictions.
Psychoanalysis is pseudoscientific quakery?
Take off points - cognitive behavioral therapy
NPR radio clip: “Cognitive Behavior Therapy: Thinking Positive”
“… Most Cognitive-Behavioral therapies are a blend of behavioral techniques and cognitive techniques—hence the name Cognitive-Behavioral—and so they do involve some amount of thoughtful awareness. Still, this sort of awareness does not need to be extensive. You could compare it to learning to drive a car and stopping at a stop sign simply because you tell yourself that if you don’t stop you run the risk of being pursued by the police and fined. There’s some philosophical processing going on here, but it’s not necessarily very sophisticated. And so, in the same way, learning to take deep breaths when angry, for example, is relaxing, but it’s a relatively simple process.
In contrast, and using the example of driving, psychodynamic psychotherapy is a bit like learning to drive by developing the understanding of the reason for stopping at stop signs (that is, the need to be cautious when entering any intersection lest you collide with something) and also you extend this basic reason to other behavior (that is, you learn to look beyond “simple” behavior into its motives and consequences—for example, you come to understand the need to begin a trip by planning the route and checking the gas and oil, rather than just turning the key and going). And so you learn, when feeling angry, for example, to track the anger back into similar earlier experiences and feelings, many of them previously unconscious; thus you come to understand the components of your current feelings, and you are enabled to take actions with full awareness of the origins and consequences of your motives.
Many people want nothing more than to “turn the key and go,” and to watch out for police along the way. It’s your choice.”
“For people with mental illness, psychotherapy affects the brain’s neural networks in much the same way that medicines do, according to Ari Zaretsky, M.D., head of the Cognitive Behaviour Therapy Clinic at Sunnybrook and Women’s College Health Sciences Centre and an assistant professor of psychiatry at the University of Toronto.
"Many people view psychotropic drugs as the potent interventions, as if they are the biological intervention and psychotherapy is not," said Zaretsky.
Zaretsky presented evidence that different forms of psychotherapy can alter the brain’s processes for patients with different types of psychiatric disorders in much the same way that antidepressants do.
For those with psychiatric illnesses, the "experiential learning" from cognitive-behavioral therapy (CBT) has been shown to alter some of the same biological mechanisms typically affected by medications, Zaretsky said.”
“It is bad enough to be depressed because of difficult living circumstances or to be anxious because you are subjected to regular domestic violence, without being told your depression or anxiety are caused by your own dysfunctional cognitions. Blaming the victim like this imposes irrelevant therapeutic rituals on top of societal oppression”
Changing politicians' minds about changing our minds?, UK Community Psychology network


Comments
thoughts..
Psychotherapy plus ...
Rich conversation last Monday night and here. Glad to have it noted, appropriately, that Freud/psychonanalysis remain relevant, despite social/cultural fads (more in the US than in Europe, for example), and think the situating of CBT somewhere between dynamic psychotherapy and pharacotherapy makes sense. Think as well it makes sense not to debate the merits of different therapies in the abstract but instead to note that they seem to have different underpinnings and may each prove useful in one or another set of circumstances. For what its worth, Freud developed the position that psychoanaysis might best be thought of not primarily as a therapeutic procedure for particular problems but rather as an empowering mechansim for anyone. Glad too to have the loop through culture appropriately and usefully noted. I'm myself intrigued by the idea that not only are all mental health problems related to story telling but that a major subset of them have to do with the centrality of story in interpersonal relations.
Like others, I too heard the issue of how to think about discomfort/pain in a mental health context as a major theme of our Monday conversation and that discussion seems to me to have been usefully extended here. For more on my evolving thoughts along those lines, see "illness as metaphor revisited" and "an alternative to fight and flight." Relief of pain/discomfort should certainly be a consideration in mental health but not at the price of abolishing generative conflict. To put it more positively, the objective should be to facilitate the brain's ability to use conflict creatively and this may at times depend on reduction of pain/discomfort. The latter is not the sine qua non of therapy but can be a valuable aid. One may think of this as a difference from the "medical model" approach, or, alternatively, as a needed feature of that approach as well.
Along these lines, Julia challenged me on my suggestion that epilepsy is a one-time "mental health" phenomenon that is now well enough understood to have been reclassfied since it has little or no "story" component. And, depending on how one defines things she's right.
NEAD = "non-epileptic attack disorder." So, 1 in 5 people with behavioral symptoms that would have been called "epilepsy" several decades ago ... don't have "epilepsy" in the sense that they are not helped by existing treatments for epilepsy. I can't help but wonder what they do have, and what the role of story telling might be in it.
Also had some thoughts about a "good therapist", ie what the "professional skills" are that result in something more than one can get from a good friend ...
Finally, for those of you waiting breathlessly, here' the results of our Monday survey . Values in the table are numbers of the eighteen people present for the discussion whose experience with pharmacotherapy and talk therapy is as described in the table heading. Better than 80% of us have some experience with one or another form of mental health procedure. It would be interesting to know how these compares to other groups of people, both today and in the past.
Story of an Injured Storyteller
Me: “Did I black out?”
KC: “No I started talking to you right away and you responded.”
Me: “Really, what did we talk about?”
KC: “You don’t remember?”
Me: “No, I remember sitting up and you explaining that you couldn’t come closer. I wondered how you managed to catch my pony too.”
Upon closer examination, I found sand and/or bruising on my right elbow, shoulder, back, and the back of my helmet. Some physical evidence that I did indeed hit my head. Some physical symptoms that I experienced were blurry vision, headache, and light and sound sensitivity. All this evidence is consistent with a grade II concussion, confirmed by Bryn Mawr Hospital ER. Concussion is generally defined as a temporary loss of brain function. Its most common symptom is memory loss; however, loss of consciousness only occurs in severe cases.
According to my trainer, KC, I sounded just like myself, for those five minutes immediately after the fall. We chatted about my fall, and how well I rolled away. Yet I have no recollection of that time period. My storyteller was not functioning; it did not generate memories of those scenes. This reminded me of our class discussion of sleepwalking and associated phenomena.
A concussion is an injured storyteller in our terminology. What does an injured storyteller do? Park cars sideways in straight spots? Mumble nonsensical responses? Not communicate, control, or monitor the unconscious? This is how a concussion can feel like mental illness.
Etc.
I think much of the isolation stems from having removed experience from a context in which pain, grief, disappointment, anxiety etc. are common experiences, shared experiences to varying degrees. The move towards an embrace of ever narrower definitions of “normal” and a diminished sense of interpersonal connections has led to more social isolation, an increased sense of isolation in one’s experience, when, in actuality, that experience is not so “different” after all. The logical end to this particular paradigm is to seek a “cure,” not to respond to the challenges and opportunities presented by such an experience. We have reached a place, collectively, where our bodies (yes, our minds, too) are seen in times of duress as the enemy. Illness happens to us, but is not a part of us. And for some, this may be a useful way in which to construct an experience of illness, to be apart from it and address it as an outsider. For others, however, this may lead to increased alienation and difficulty responding to the challenges and potential gains to be made when mental health is in flux. Surely, health and mental health are not products of simple cause and effect relationships, and perhaps should not unto themselves be a goal. The very language of "illness" and "health" seems to exist not along a continuum but as an all or nothing, defined set of milestones and endpoints that undermines individual, nuanced experiences and catapults illness into the realm of battle: doctor vs. unruly body. I think this framwork is limited and in some cases detrimental. However, I maintain that bringing nuance into the conversation does not necessitate abandoning psychotropic medications, for example, that have, indeed, made the difference for many between living in a deep, dark, hole and the ability to be a part of the world in ways that one might desire. I see therapy, whether psychodynamic, CBT or anything in between, as a way to further understand one's experience of herself in the world, her place in the world...
illness as metaphor revisited
Interesting resonance to Illness as Metaphor and AIDS as Metaphors by Susan Sontag.
Maybe the key here is not to deny "illness," in the sense of discomfort/pain and the wish to get beyond it, but rather a need to strip illness of many of its cultural (and personal?) metaphors? Or, perhaps better, to find alternate metaphors/stories ("an alternative to fight or flight"?) that derive more from "individual, nuanced experiences" and better provide "a vision of something other than what one is experiencing"? With that being a desideratum not only for "mental" health but "physical" health as well? Sontag's essay is a consideration principally of cancer, turberculosis, and AIDS.
http://www.apa.org/monitor/2
http://www.apa.org/monitor/2008/11/storytelling.html
An interesting article on autobiographical memory in this month's monitor on psych. thought it was quite perrtinent to the conversation going on in our class. Hope you all are having a great weekend.
I keep feeling like I
I keep feeling like I haven't had much to say about the past couple of topics. Who am I to say that any one therapy is ineffective or even inefficient? Who are we to say that one is better than any other? Do we even have a definition about what a "better" therapy would be? Is it cheaper? Quicker? Gets people off drugs faster? Do the patients "feel" better? I have no answers for these kinds of questions, and I haven't heard a cohesive argument from the class as of yet. The debate between CBT, pharmapsychotheraphy and psychoanalysis and any other form of therapy seems irrelevant. It's good to talk about them, I suppose, so that we know what's out there, but I don't think we can truly debate their merit. If they help even one person, however that person defines "help", then I think they have accomplished the goal they set for themselves.
I though class on Monday was
"Metaphors Matter"
To continue with the culture thread, with Merry2e's thoughts on "listening to depression," and following up on a conversation I ad with Dr. Grobstein today, here are some thoughts from writier Siri Hustvedt regarding her "battle" with migraine...thoughts which I think apply to our conversation here:
"Chronic headaches are my fate, and I have adopted a position of philosophical resignation. I am aware that such a view is resoundingly un-American. Our culture does not encourage anyone to accept adversity. On the contrary, we habitually declare war on the things that afflict us, whether it’s drugs, terrorism, or cancer. Our media fetishizes the heart-warming stories of those who, against all odds, never lose hope and fight their way to triumph over poverty, addiction, disease. The person who lies back and says, “This is my lot. So be it,” is a quitter, a passive, pessimistic, spineless loser who deserves only our contempt. And yet, the very moment I stopped thinking of my condition as “the enemy,” I made a turn and began to get better. I wasn’t cured, wasn’t forever well, but I was better. Metaphors matter."
Sometimes, though, there is an enemy--and sometimes battles can be fought and won. Which battles are worth fighting? Only those where the enemy is clearly known and where a strategy to win is clearly attainable, at little cost? When are risks and costs in battle worth bearing? When is it appropriate to resign oneself to one's condition? Can a sufferer only successfully resign oneself to his or her situation after a long, unsuccessful battle? And will that resignation necessarily bring relief or healing? Perhaps a product of my culture, I like a good fight, don't easily give up or give in, and wonder where to settle on all of this.
Fighting
Thank you for sharing that qoute and your thoughts to it. This post really helped me clarify what I mean by "Spiritual Growth" in relation to illness.
To me accepting something does not mean being resigned to it, rather it means having a different realtionship to it.
Can we learn to accept the presence of difficult circumstances (pain, depression, heartache) in our life without being resigned to their permenance?
In my life - the times when I was able to fully accept a difficult condition as it was - I found that I often had a much easier time seeing the condition clearly and beginning to work with it in a constructive way.
In contrast when I vowed to battle something to fight through, it seemed that my aversion to that thing actually kept me locked into a struggle with it.
Told from the perspective of the bipartiate brain, I think the story might look like this.
If we try to exert the will of the story-teller upon the unconscious brain and the body - without first really listening to the unconscious brain and the body we end up with a longer and more painful conflict.
If in contrast we take time and really allow all of the information from the unconscious brain to be processed in new ways we might have access to new and different stories that didn't exist before.
I am not suggesting that if you have a broken leg you sit around for months feeling the pain and trying to accept it and form a new relationship with it. However in the case of back pain - I think very often people struggle mightly against their bodies instead of learning to feel and understand the pain and learn from it.
With emotional pain, anxiety and depression, my sense is that our first instinct is to fight it, but sometimes we would do really well to start by first feeling it and then learning from it.
an alternative to fight or flight?
Since class, I have been
Since class, I have been trying to reconcile my emotions with my thoughts. It seemed to me, and still seems, that some of this talk is stigma related. Of course we grow and change through pain, of course it changes us, of course it helps us develop. Of course it is an inherent part of our life as humans, and unavoidable. Still, I truly don't think people would be as willing to suggest learning to tolerate pain that was physical or enviromental, or pain that was easily solved. Emotional and mental pain seem mysterious, perhaps always will *be* mysterious, but if there were such things as antibiotics for depression, medications that consistently worked and lightened the brunt, would we advocate avoiding them? And if there never can be, well, let's just do our best with what we have.
Here is how I can reconcile the value of pain tolerance/growth through pain with mental health: Alcohol Anonymous' serenity prayer. I have heard from a few clinicians, separated both from the idea of God and of direct substance abuse, how imporant it can be for patients to be able to ask for "the serenity to accept the things I cannot change, the courage to change the things I can; and wisdom to know the difference." I think to ask for people to recognize there are no easy answers is crucial, to ask for people to accept that there will ALWAYS be pain is crucial, to ask that people try to learn that half the battle is tolerating these upsetting emotions is crucial. But I feel no more comfortable espousing a Buddhist philosophy for general treatment of mental health than I do any other religious philosophy. (Why not channel hedonists instead?)
Pain
Recent advances inbrain research have presented us with enough evidence.
Thank you for yourresponses. I am still trying to sort out where I stand on the issue of pain andthe various ways one can work with it. It’s very helpful to try to tease outsome of this stuff.
I want to clarify, thatI actually don't make a distinction in this case between physical and emotionalpain. I think that in both cases a better distinction is the one that we raisedin class - the difference between acute and chronic pain.
I will try to use myselfas an example (with awareness of all the biases that introduces). 5 yearsago I had a hip replacement. The hip replacement was needed because a childhoodinfection had destroyed the head of my femur. Walking had become increasingly painful.Since the replacement, I have had no pain in my hip, but I have developed lowerback pain from walking. While I would certainly be a candidate for painmedication - I choose instead to use the lower back pain to guide myrehabilitation and attempt to make my body work better.
I don't do this becauseI am a masochist and enjoy pain. I do this because I think the tightness in mylower back is directly related to things that I can change in the way I walk,exercise, stretch, etc, that will improve my life. Generally I think the paincan show me something meaningful in my attempt to get healthier.
My own sense isthat things might work similarly in emotional pain.
Again let me be clear. Iam not against emotional pain medication. But I think that anti-depressants akenover years seem to function more like pain killers than like anti-biotics. Doesthat make them "wrong" or "bad" in my perspective? No.
I just think it’shelpful to examine both the advantages and pitfalls of dealing with chronicemotional and physical pain in this way.
I appreciate what you added
sorry, another culture post
Paul mentioned culture in class again this week which is an aspect of the mental health debate I find particularly interesting. Talk therapy, as we know it, is a relatively modern phenomenon and alot of people may view it as especially indulgent and elitist. Surely we existed thousands of years on the earth without having to discuss how, for example, my relationship with my father might or might not affect relationships I have with men. However, this arguement ignores a crucial difference between this time period and the experiences of humans before. In this sense, I am not talking about certain illnesses like schizophrenia, but problems such as depression, anorexia and anxiety.
Our culture has changed dramatically and so have the ways in which we interact with eachother. We live increasingly isolated lives, in communities that no longer interact in the same ways they used to. Perhaps for that reason, interpersonal relationships take on a new kind of significance since we have lost the kinds of connections we used to have.
Undoubtedly there are people in say, the third world, who have mental illnesses like bi-polar disorder or depression. Arguably however, diseases such as Anorexia occur amongst predominantly western populations. It may appear that mental health and mental health issues have become something of a 'fad'. However, the change may be occurring in the bigger picture, the nature of our modern culture means that we have to deal with issues that did not effect us in the past.
We have existed for thousands of years
I want to second akerle's comments.
I always find the "we have existed for thousands of years without" argument to be specious. You don't hear intelligent people talking about how we existed for thousands of years without electric toothbrushes, x-rays, telephones and uninvasive hip replacements.
The discussion should always be more nuanced. We have to talk about the ways that a given innovation has improved our lives as well as the things that it may have cost us. This type of discussion - will help frame individual innovations in a larger cultural context.
If we approach talk therapy in this way - its clear that it has been a tremendous help to many people who suffered greatly. It is less clear to me that it has significantly weakened social structures.
Rather it seems as pointed out above that social structures - for good and for bad have been eroded by modernity and city life. We have significantly more freedom and that freedom - can be both very helpful for people (especially people who do not "fit in") but it can also prove to be very isolating to people.
If anything it seems that good talk therapy is trying to help people cope wtih a new situation of big, open societies where people are free to make their own meaning - instead of having meaning and order imposed upon them by religious and social structures.
One can make the argument that we have lost something due to this increased freedom. It would be interesting to discuss how societies can find ways to create more sense of community and keep people from becoming desperately isolated.
It's funny ... We ended
It's funny ...
We ended class with the quote on how CBT could be used to invalidate people's thought processes ... In the NYTimes today there is an article on how the internet has made room for online communities where people can share stories of governmental stalking/mind-reading (Sharing Their Demons on the Web) and it has doctors discussing the merits and problems with this ... The importance of social support, and the forging of relationships (it mentions how the group component of CBT can be important), while also encouraging these faulty cognitions.
At this moment, CBT seems like a rather unnuanced cruel form of treatment. One of those things you know works, but can't quite get your mind around.
This week inspired some
This week inspired some thoughts about the relationship between personality and therapy. Pharmacotherapy and talk therapy provide us with a tools that may be more useful for some individuals than others. For example, individuals with clearly defined problems that they wish to address can appreciate the brief, cheaper, and more targeted approach of CBT. However, others are incapable of articulating a specific problem. That doesn’t mean that they don’t deserve help, need help, or are ready for help. It is possible that they are seeking professional help because of an inability to resolve dissatisfaction with their mental states through informal routes. Their lack of communication can be considered a symptom of their mental illness.
Returning to considerations about who makes a good therapist. For psychoanalytic psychotherapist a lot of patience is necessary to be able to appreciate the therapeutic process. In her book, “The Drama of the Gifted Child,” Alice Miller theorizes that only people who have suffered are interested in being psychoanalysts. She also states that a “therapist’s sensibility, empathy, responsiveness, and powerful “antennae” indicate that as a child he probably used to fulfill other people’s needs and repress his own.”
Initial thoughts
I'm glad we got to spend a little time talking about Freud and psychoanalysis on Monday. As Dr. Grobstein pointed out, the man and his thoughts are such a huge influence on pretty much everything we talk about in class every week.
I had a professor in undergrad who always referred to Freud as Sigmund "Fraud," and who was fond of saying, "Now, now, its not true that Freud did enough cocaine to kill a small horse. (pause) No, Freud did enough cocaine to kill a large elephant." Although this was somewhat funny, it never really sat right with me. I know a lot of Freud's theories (Oedipal complex) have fallen out of style, but a lot of them are still valid and in use today (defense mechanisms). So, calling it a social nuisance (Marty's third quote) is not doing justice to the pioneering Freud did.
As far as a comparison between CBT and psychoanalysis, I don't see much difference in the end goal - to develop a new story. It seems like CBT just gives you a more concrete method for doing this. More tools... It seems empowering to me.
With that in mind, I disagree with Yona and Katy's final quote. If you were blaming the victim, then I suppose that would not be constructive, but that was never my impression of CBT. To me, it seemed like the patient was made aware of harmful cognitions, but not blamed for them.
Lastly, I've been thinking about Adi's question about the usefulness of sadness in a spiritual context. Considering the content of our discussions this semester, I'm hesitant to assign any significance or purpose to sadness as helping move along a spiritual path because it would follow that there is an end to that path or a final goal we are working towards. I still feel like there is no external greater meaning to things beyond the meaning that is assigned by our storytellers.
However, I was reading about physics (astronauts in particular) and I started thinking about this again. When astronauts are in space, one of the dangers that they have to worry about is the fact that there is no gravity in their space shuttle. As a result, their muscles atrophy. If we took away sadness, using medications or any other means, then there is little doubt in my mind that some part of us would atrophy. I just hesitate to say whether this is "good or bad."
Genes and "underlying causes"
The nytimes science section has a whole bunch of really interesting articles today about genetics and mental illnesses! This one I like in particular, and I think speaks to a lot of what we discussed about how much of who we are is preprogrammed into us vs the idea that our "genes" are nothing until they are read and acted upon by the body:
One scientist from the article says (about DNA) “it doesn’t do anything by itself.” It is a profoundly relational molecule, she said, and it has meaning only in the context of the cell. To focus endlessly on genes, she said, keeps us stuck in a linear, unidirectional and two-dimensional view of life, in which instructions are read out and dutifully followed."
http://www.nytimes.com/2008/11/11/science/11angi.html?pagewanted=1&ref=science
Enjoy!
Brain variation and story telling?
Yep, the whole section is worth looking at. Including an article about some new work suggesting that the autistic spectrum - "a fascination with objects, patterns, mechanical systems, at the expense of social development" is at one end of a continuim of brain variations with "the psychotic spectrum ... hypersensitivity to mood, their own and others' ... schizophrenia ... as well as mood problems" at the other. See In a novel theory of mental disorders, parents' genes are in competition. Whether the genetics plays out as suggested or not, there is an interesting new approach to characterizing brain variation here. Different styles of story telling?
For more on genetics, see the 7 November 2008 issue of Science, a special issue on Genes and Behavior, including a review on Genes and Social Behavior.
Depression as a "settling embrace"?
If society stopped
Merry2e, I think if society actually stopped and allowed itself to feel, to be, we might learn that many of the things that we think are the most important things in life, aren't. Conversely, we could learn that we don't give enough recognition of and attention to the things that in the end, just may be the most important things in life. I'll hold back giving any examples--it's more meaningful and interesting if you come up with them on your own. df
Listening to depression
I spoke with a wise person this evening before class about the topic of depression. Should one drive themselves through it, trying to get to the other side? Meds? Therapy? Or how about staying still and listening to the depression and actually feeling and listening to it? The discussion in class and with the wise person reminding me of a book that was collecting dust on my bookshelf.
"Sometimes, into the lives of women who seem to be successfully fulfilling the standards of the surrounding society, depression may come as a settling embrace. It may come to a woman who is terrified that there will be nothing there, inside, if she allows herself time to rest, to seperate from her extraverted hyperactivity in the outer world. [...] Into such a life, depression comes as a gift, bringing the chance to strike root in a deeper ground inside oneself. Depression comes as a gift forcing one to listen to the voice of the Self within." (p.65)
(Duerk, Judith. Circle of Stones: Women's Journey to Herself. Inner Ocean Publishing, 1989.)
I wonder what would happen if we as a society actually stopped. Just stopped and allowed ourselves to feel, to be. What could we learn?
Post new comment